MALE INFERTILITY
Infertility is medically defined as the inability to conceive following one year of regular sexual intercourse without contraception or after six months if the woman is over age 35.
There are two general types of infertility.
- Primary infertility is defined as difficulty conceiving for a couple who has never before had a child.
- secondary infertility describes a couple who is having difficulty conceiving when at least one of the partners has previously had a baby.
It is a medical condition faced by around 10% of the couples.
It is caused by both Male and Female factors. Male factors in about 40% of the cases, female factors also in about 40% of the cases are responsible for infertility. Whereas in nearly 10% of the cases, both factors are responsible and in 10% of the cases, no obvious factors can be found – unexplained infertility.
Female factors are discussed elsewhere in this website.
Here we will see the Male factors Infertility.
Causes of Male Infertility :
A variety of disorders ranging from hormonal disturbances to physical problems, to psychological problems can cause male infertility. Although many treatment options are now available, in many cases treatment will not work. In many instances, male infertility is caused by testicular damage resulting in an inability of the testicle to produce sperm. Once damaged, the testicle will not usually regain its sperm-making capabilities. Despite medicine’s limited ability to treat male infertility, many successful treatment options are available for its many causes. Besides testicular damage, the main causes of male infertility are low sperm production and poor sperm quality.
1. Life style : fertility reflects a man’s “overall” health. Men who live a healthy lifestyle are more likely to produce healthy sperm.
The following list highlights some lifestyle choices that negatively impact male fertility
• Smoking significantly decreases both sperm count and sperm cell motility.
• Prolonged use of marijuana and other recreational drugs.
• Chronic alcohol abuse.
• Anabolic steroid use causes testicular shrinkage and infertility.
• Overly intense exerciseproduces high levels of adrenal steroid hormones which cause a
testosterone deficiency resulting in infertility.
• Inadequate vitamin C and Zinc in the diet.
• Tight underwear increases scrotal temperature which results in decreased sperm production.
• Exposure to environmental hazards and toxins such as pesticides, lead, paint, radiation, radioactive
substances, mercury, benzene, boron, and heavy metals
• Malnutrition and anemia.
• Excessive stress!
2. Hormonal Factors : The hypothalamus-pituitary endocrine system regulates the chain of hormonal events that enables testes to produce and effectively disseminate sperm. Several things can go wrong with the hypothalamus-pituitary endocrine system. High level of Prolactin hormone, Low level of Thyroid and Gonadotropins are main hormonal causes.
3. Physical factors : Testes are placed in scrotal pouch outside the abdomen because they need lower temperature than body to function properly. Any condition that increases the temperature around the testes can result into less function of testes causing low sperm count and low motility of sperms.
a. Working in high temperature area : working in places where high heat is generated like furnaces, kitchen etc..can cause drop in sperm production.
b. Use of very tight and synthetic clothing : this prevents proper ventilation around the testes and keeps them in constant touch with high temperature of abdomen.
c. Exposure to frequent Sauna, Steam : increases local warmth and impair sperm production
d. Varicocele : A varicocele is an enlargement of the internal spermatic veins that drain blood from the testicle to the abdomen (back to the heart) and are present in 15% of the general male population and 40% of infertile men.
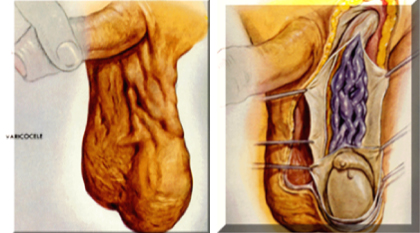
A varicocele develops when the one way valves in these spermatic veins are damaged causing an abnormal back flow of blood from the abdomen into the scrotum creating a hostile environment for sperm development. Varicocoeles may cause reduced sperm count and abnormal sperm morphology which cause infertility.
Variococles can usually be diagnosed by a physical examination of the scrotum which can be aided by the Doppler stethoscope and scrotal ultrasound.
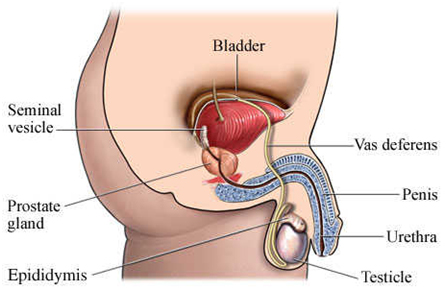
4. Defective sperm passage : Nearly 7% of the cases may have sperm transportation problems. After being produced in testes, sperms are transported thru Epididymis, seminal vesicle and ejaculatory duct. This pathway of sperms may be blocked by many factors like.. absence of vas deference since birth, genetic defects or scarring of the ducts following infections like Tuberculosis (TB) and Sexually Transmitted Infections (STIs).
5. Testicular Atrophy : sometimes the testes get damaged and they stop functioning and reduce in size. This is known as atrophy. Sometimes infections like Mumps, tuberculosis, brucellosis, gonorrhea, typhoid, influenza, smallpox, and syphilis can cause testicular atrophy. Atrophy results in zero sperms in semen.
6. Undeveloped Testes : Sometimes, one or both testes fail to develop after puberty. Non-descended testes always remain non-developed and results into zero sperms.
7. Retrograde Ejaculation: Is a condition in which semen is ejaculated into the bladder rather than out through the urethra because the bladder sphincter does not close during ejaculation. If this disorder is present, ejaculate volume is small and urine may be cloudy after ejaculation.
8. Sexual Dysfunctions : following sexual dysfunctions can cause Infertility..
9. Erectile Dysfunction : Inability to achieve or maintain Erection sufficient for Intercourse is known as Erectile Dysfunction. There are many causes for this problem both physical and psychological (discussed in detail elsewhere). Most men who suffer from ED have a secondary psychological problem that can worsen the situation like performance anxiety, guilt, and low self-esteem.
For many couples, sex becomes a mean to attain fertility only and not for pleasure. They loose the spontaneity in sex. Many men become very much conscious during the ovulation period of wife because often they are advised by the doctors to have sexual intercourse for fertility. Under pressure, they fail to attain good erection and fail miserably.
a. Premature ejaculation (Early ejaculation) : Premature ejaculation becomes a fertility problem when ejaculation occurs before a man is able to fully insert his penis into his partner’s vagina.
b. Ejaculatory Incompetancy (absent ejaculation) : This rare psychological condition prevents men from ejaculating during sexual intercourse even though they can ejaculate normally through masturbation. Often these men have high threshold for ejaculation (Opposite to premature ejaculation where the threshold is low.) and sometimes it is a result of performance anxiety. Similarly, Many men can not even masturbate and hence can not give semen sample in the laboratory for testing.
HISTORY TAKING in Infertility :
1. Duration : of marriage
2. Trying time : for pregnancy
(Duration of marriage is not the same as ‘Trying time’)
3. Sexual History :
a. Potency and penetrative sex
b. Orgasm and Intra-vaginal orgasm
c. Use of Lubricants
d. Timing of intercourse (with reference to intercourse)
e. Does wife douche immediately after intercourse?
f. Frequency of Intercourse
4. Childhood and Development :
a. Undescended testes
b. Testicular trauma, torsion, inflammation
c. Onset of puberty
5. Surgical history : any previous uro-genital surgery
6. Medical history :
a. Infections : viral fever, mumps, sexually transmitted infections (STIs), small pox, Tuberculosis (TB)
b. Toxins and Drugs : exposure to chemicals, heat, radiation. Drugs like tobacco, alcohol, steroids, chemotherapeutics etc...
INVESTIGATIONS for MALE INFERTILITY
Investigations are confusing, time consuming and often expensive. It is not an easy task. It should have a systematic approach without which a couple may lose the right direction and may be lost in the maize of various tests and may find it very cumbersome, tedious and disappointing.
If the couple is not counselled properly at the various stage of the investigations and treatment, they may remain wondering about the outcome of the treatment.
Frequent changing of doctors and center will also confuse the couple and often leads to the repeated investigations which may not lead them to any particular direction.
Following are the list of investigations. The doctor will not carry out each and every test for all the couples but depending on the individual case, the appropriate tests need to be done.
1. SEMEN ANALYSIS : This is one of the most important test to be performed for male infertility. It is an easy, convenient and non-expensive test which gives nearly 70 % of the evaluation of the male infertility.
In fact, in most cases, semen analysis should be done prior to any female investigations because first attending male factors in infertility makes it easy for female evaluation.
Around 10% of men may not find it easy to give semen sample in the laboratory because...some have never masturbated, some are inhibited in the crowded laboratory and may not get aroused in the filthy washrooms to masturbate whereas some men often become nervous to masturbate ‘on demand’.
Failure to give semen sample in the laboratory can be very disheartening and embarrassing for a man and can prolong long delays in treatment. Person should be instructed properly and if there is a difficulty then, he can try collecting it at home (partner’s help can be taken). Collection in condoms is to be avoided because most condoms are spermicidal means sperms lose their motility in those condoms. Special non-spermicidal condoms can be used. In more difficult cases, penile vibrators and electro-ejaculators can be used to facilitate ejaculation.
Semen Analysis : Normal Parameters
VOLUME : more than 1ml
SPERM COUNT : more than 20 mill per ml
MOTILITY : more than 50% forward progressive or more than 25% rapid progressive
MORPHOLOGY : more than 30% normal
VITALITY : more than 75% alive
Many pathological laboratories still quote the old norms which are misleading and causes un-necessarily nervousness in the infertile couple.
If the routine Semen Analysis shows, presence of pus cells, then, SEMEN CULTURE needs to be performed to find the nature of infectious organisms.
In some cases, SPERM FUNCTION TESTS needs to be carried out.
Following are some of the important Sperm Function Tests (SFT) :
1. Hypo-Osmotic Swelling Test : this test is a good indicator of healthy spermatozoa
2. Acrosome Test : this test indicates sperm’s ability to penetrate the female egg.
3. Nuclear Chromatin Decondensation Test : indicates sperm’s maturation
4. Sperm Mitochondrial Activity Index : helps to understand the sperm motility.
POST COITAL / CERVICAL MUCOUS TEST : This is supplementary test of Semen Analysis where the sperm movement in the woman’s vagina is examined as it checks the compatibility of a man’s sperm with the mucus of his partner’s cervix.
If the sperm and mucus are incompatible, the sperm is unable to pass through the mucus into the fallopian tubes and fertilize the egg.
2. HORMONAL TESTS : measures blood levels of the hormones involved in sperm production like Follicle Stimulating Hormone (FSH), Luteinising Hormone (LH), Prolactin (PRL) and Testosterone.
3. SONOGRAPHY : of scrotum would be necessary to diagnose the Varicocele
4. SPERM ANTIBODY TEST :
5. TESTICULAR BIOPSY : this is a minor operative procedure where a small piece of testicular substance is removed and is tested to check the sperm production process. This is advised to the men who have zero sperm count (Azoospermia). Presence of sperms confirms the production. It is also carried out to extract and collect few sperms which can be used for IVF (test tube baby treatment).
6. GENETIC TESTS : Tests like Karyotyping (Chromosome study) may be required to confirm certain Genetic conditions
TREATMENT of MALE INFERTILITY
After basic optimum evaluation, therapy for Oligo-astheno zoospermia should start.1. Basic Treatment :
• Balanced Diet, moderate exercise, avoiding Smoking, Alcohol, drugs etc are to be employed to keep oneself in good health.
• Avoid excessive heat exposure, loose cotton underwears, avoiding Sauna, Steam will help improve the sperm count
• Therapy for stress relief
2. Medical Treatment: a sperm cell requires approx 72 days to become a mature sperm from the germinal cells. Hence, medical treatment requires patience. Minimum therapy cycle that should be tried is about 3 months. Discontinuing or changing the treatment in between will result into loss of both time and money.
• Empirical treatment: Anti-oxidants like vitamin E, L - Carnitine, Lycopene, Coenzyme Q 10 etc. are beneficial but at variable level to different persons. Zinc and selenium containing multivitamins may also be useful.
• Clomiphene Citrate : it can stimulate the pituitary of the brain to release hormones which will stimulate sperm production
• Human Menopausal Gonadotropins (HMG) and Human Chorionic Gonadotropins (HCG) are useful in cases where the hormone levels are lower than the required normal levels.
• Antibiotics : given when there is infection in seminal vesicle or prostate.
• Steroids : given for the treatment of anti-sperm antibodies.
3. Surgical treatment : following surgical treatment is available.
a. Varococele ligation : this option should be considered when the sperm count is not improved with initial trial medical therapy. Surgery can be beneficial by about 60%. Diagnosis should be confirmed by Sonography.
Varicocele surgery should be performed by Microsurgical ligation.
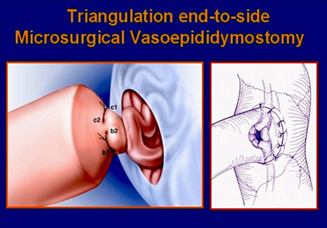
b. Vaso-Epididymal Anastomosis (VEA) and Vaso-Vasal Anastomosis (VVA) : this is the surgery carried out to remove the block in the sperm passage. This is one of the most delicate surgeries which is done under microscope requires good experienced surgeons. Indicated for those men who have undergone vasectomy but wants it to be reversed to have more children.
c. SPERM RETRIEVAL TECHNICS : if for one or more reasons, if the block removal fails, then sperms can be retrieved from the men’s reproductive organs thru following methods and subsequently that can be used for IVF (Test tube baby) treatment.
• Micro Epididymal Sperm Aspiration (MESA)--involves a delicate surgical technique that utilizes a microscope to get a sperm sample from epididymis
• Percutaneous Epididymal Sperm Aspiration (PESA)--a small needle is used to aspirate sperm from epididymis
• Testicular Sperm Biopsy (TESE)--a small biopsy of testicular tissue is taken and a sperm sample is removed from the biopsy.
4. Assisted Reproductive Techniques (ART) : for oligospermia, following ART options are available.
• Intra Uterine Insemination (IUI) : useful in cases where the sperm count is more than 10 mill/ml. Success rate upto 25% per attempt.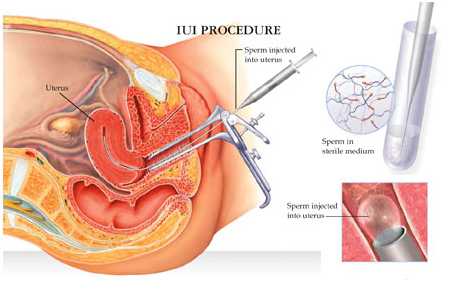
• Intra Cytoplasmic Sperm Injection (ICSI) : this has revolutionised the management of very severe low sperm count and even Azoospermia.
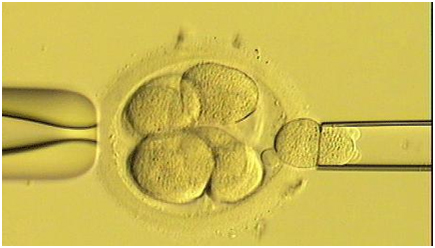
ICSI involves the injection of sperm directly into the ovum. Only a single sperm is needed in ICSI, hence, poorly motile sperm can also be used.
Many couples are reluctant to use ART thinking it to be an expensive treatment and waste much time and money on other procedures repeatedly. Instead, if focused attempts are made for Art, then it might give better hope.
5. Donor Insemination : When a man has Azoospermia due to testicular failure which can not be treated, Donor Insemination is suggested. This involves procurement of healthy sperm from physically and psychologically healthy donor and after thorough testing, it is inseminated artificially thru minute syringe by a qualified doctor.
This is a legal treatment option. Treating doctor MUST maintain absolute anonymity of donor and recipient couple from each other. This means that donor should not know who the recipient is and recipient should not know who the donor is. DONOR INSEMINATION MUST BE AVOIDED FROM THE DONOR KNOWN TO THE COUPLE to prevent future emotional and relational complications.
Humour in sex





