FEMALE INFERTILITY
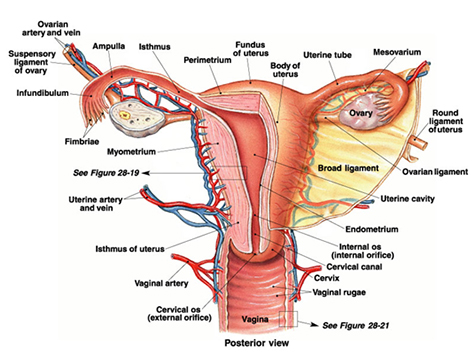
Female Sexual Anatomy :
Infertility is medically defined as the inability to conceive following one year of regular sexual intercourse without contraception or after six months if the woman is over age 35.
The definition also includes women who are unable to carry a pregnancy to live birth.
There are two general types of infertility.
• Primary infertility is defined as difficulty conceiving for a couple who has never before had a child.
• Secondary infertility describes a couple who is having difficulty conceiving when at least one of the partners has previously had a baby.
It is a medical condition faced by around 10% of the couples.
It is caused by both Male and Female factors. Male factors in about 40% of the cases, female factors also in about 40% of the cases are responsible for infertility. Whereas in nearly 10% of the cases, both factors are responsible and in 10% of the cases, no obvious factors can be found – unexplained infertility.
Male factors are discussed elsewhere in this website.
Here we will see the female factors Infertility.
Normal Female Reproductive System :
Causes of Female Infertility :
1. Hormonal Disorders : When the hormones like Follicle Stimulating Hormone (FSH), Leutinising Hormone (LH), Prolactin (PRL), Thyroid hormones etc. are not in balance, it disturbs the menstrual cycle pattern and can cause difficulty in ovum preparation and its release (failure to ovulation). Very severe deficiency of hormones may lead to premature menopause also.
2. Fallopian tube disorders : tubal block (obstruction) and adhesions are responsible for about 25% of female infertility. The block may be the result of infection, birth defects, abdominal surgery or the ectopic pregnancy.
The block does not allow the ovum and the sperm to unite with each other.
3. Endometriosis : it is presence of endometrium at abnormal places like tubes, ovaries and peritoneum etc... often, it is the inadequate thickness of endometrium is the cause for the problem
4. Cervical factors : Approximately 3% of couples face infertility due to problems with the female ís cervical mucus. The mucus needs to be of a certain consistency and available in adequate amounts for sperm to swim easily within it. The most common reason for abnormal cervical mucus is a hormone imbalance, namely too little estrogen or too much progesterone.
5. Uterus abnormality : about 10% of the cases. Fibroids, poplyps, adenomyosis etc can cause obstruction and some birth defects (congenital abnormalities) like septate uterus, bi-cornuate uterus etc will not allow the conception in the uterus.
6. Life Style : It is well-known that certain personal habits and lifestyle factors impact health; many of these same factors may limit a couple's ability to conceive. Fortunately, however, many of these variables can be regulated to increase not only the chances of conceiving but also one's overall health.
Diet and Exercise : Optimal reproductive functioning requires both proper diet and appropriate levels of exercise. Women who are significantly overweight or underweight may have difficulty becoming pregnant.
Smoking : Cigarette smoking has been shown to lower sperm counts in men and increases the risk of miscarriage, premature birth, and low-birth-weight babies for women. Smoking by either partner reduces the chance of conceiving with each cycle, either naturally or by IVF, by one-third.
Alcohol : Alcohol intake greatly increases the risk of birth defects for women and, if in high enough levels in the motherís blood, may cause Fetal Alcohol Syndrome. Alcohol also affects sperm counts in men.
Drugs : Drugs, such as marijuana and anabolic steroids, may impact sperm counts in men. Cocaine use in pregnant women may cause severe retardations and kidney problems in the baby and is perhaps the worst possible drug to abuse while pregnant. Recreational drug use should be avoided, both when trying to conceive and when pregnant.
7. Environmental and Occupational factors : The ability to conceive may be affected by exposure to various toxins or chemicals in the workplace or the surrounding environment. Substances that can cause mutations, birth defects, abortions, infertility or sterility are called reproductive toxins. Lead, Ethylene oxide, X ray radiation & chemotherapy and Dibromochloropropane (DBCP) found in pesticides can cause ovarian problems, leading to a variety of health conditions like early menopause that may directly impact fertility.
INVESTIGATIONS for FEMALE INFERTILITY
Investigations are confusing, time consuming and often expensive. It is not an easy task. It should have a systematic approach without which a couple may lose the right direction and may be lost in the maize of various tests and may find it very cumbersome, tedious and disappointing.
If the couple is not counselled properly at the various stage of the investigations and treatment, they may remain wondering about the outcome of the treatment.
Frequent changing of doctors and center will also confuse the couple and often leads to the repeated investigations which may not lead them to any particular direction.
Following are the list of investigations. The doctor will not carry out each and every test for all the couples but depending on the individual case, the appropriate tests need to be done.
1. Ovulation study : This is to determine whether the woman is ovulating on a regular basis and whether the timing of ovulation could be assessed.
Tests of ovulation may include basal body temperature monitoring (which can indicate after the fact that a woman has ovulated) and ultrasound testing (which detects the number, size, and shape of the egg follicles, follows the growth of follicles, and identifies whether follicles have collapsed, indicating that ovulation has occurred). Sometimes blood tests to determine hormone levels or an endometrial biopsy to observe the development of the uterine lining may be required.
2. Post Coital Test : to assess if there is a problem in the interaction between a woman's cervical mucus and her partner's sperm. A post-coital test necessitates the couple to have intercourse before the woman visits the physician’s office to examine her cervical mucus.
3. Imaging : test like Hystero-Salpingo-Gram (HSG) is done to visualise the uterine cavity and the patency of the Fallopian tubes.
4. Laparoscopy and Hysteroscopy : Invasive investigations may be required to assess the pelvic organs thru the endoscope which is inserted through the abdominal wall.
TREATMENT OPTIONS FOR FEMALE INFERTILITY
Drugs (Medicines) : Ovulatory disorders are involved in about 40% of fertility problems. Currently, there are two major drugs used to treat ovulatory disorders, namely human menopausal gonadotropins (hMG) and clomiphene citrate, Letrozole etc.
Human chorionic gonadotropin, for example, may be needed to trigger follicle rupture (ovulation). To support ovulation and pregnancy, progesterone may be prescribed alongside an hMG.
Other Options : also known as Assisted Reproductive Techniques (ART).
Intra Uterine Insemination (IUI), In Vitro Ferilisation IVF (Test tube baby) are the common ARTs.
Intra Uterine Insemination (IUI) : This treatment involves direct deposition of the sperms into the uterine cavity with the help of a small catheter. Here the sperms bye pass the cervical canal of the woman and the path of sperms is reduced thus trying to facilitate better availability of the sperms for fertilisation.
IUI is a non-invasive treatment option which does not require hospital admission, it does not require anesthesia and involves relatively less expenses.
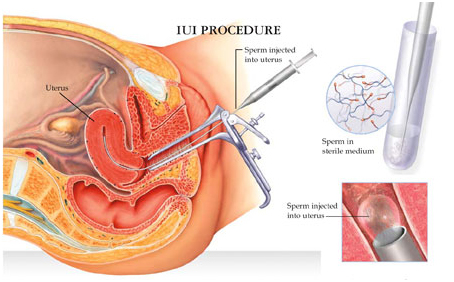
This treatment is useful in cases where the sperm counts are moderately low, cervical factors are present or in cases of unexplained infertility.
In Vitro Fertilisation - IVF (Test tube Baby): In IVF, after ovulatory stimulation, oocytes are surgically retrieved from the woman, combined with the partner's sperm in the laboratory, incubated for one to three days, and then transferred into the woman's uterus, where implantation and development of a healthy baby will hopefully occur.
This is an expensive treatment option with less success rate. However, with more advanced techniques emerging, success rate can be expected to improve.
Micro-manipulation (Intra Cytoplasmic Sperm Injection ICSI) is currently widely used technique in IVF.

Less commonly used ARTs include gamete intrafallopian transfer (GIFT) and zygote intrafallopian transfer (ZIFT). GIFT requires the woman to have a functional fallopian tube and is performed in a single procedure. The woman's eggs and the sperm are combined in a catheter and immediately inserted into the woman's fallopian tube, rather than mixing oocytes and sperm in the laboratory. ZIFT has a very poor success rate and is rarely used today.
Embryo cryopreservation is a procedure in which multiple oocytes are removed from a woman, fertilized, and then frozen for future use. This technique allows multiple transfers to occur with only one cycle of stimulation and retrieval.
Often, older women may require donor oocytes in order to become pregnant.
If none of these procedures prove successful, Gestational Surrogacy may be considered in the case of women with healthy eggs who cannot carry a pregnancy to term.
Humour in sex





